You are about to embark on a fascinating journey into the world of high-altitude medicine and physiology. In this article, we will explore the unique challenges and adaptations that occur when you venture to great heights. From the breathtaking mountain peaks to the unlikely habitats of high-altitude climbers, we will uncover the secrets of how our bodies react and adjust to the thin air and harsh conditions found at elevations above 8,000 feet. So, fasten your seatbelt and get ready to explore the wonders of high-altitude medicine and physiology!

Introduction
Welcome to the fascinating world of high-altitude medicine and physiology! As you embark on your journey to high-altitude regions, it’s essential to understand the unique physiological changes that occur in your body at these heights. This comprehensive article will guide you through the various aspects of high-altitude medicine, including physiological changes, altitude sickness, cardiovascular and respiratory effects, hypoxic training, preventive measures, medical considerations, emergency situations, and future perspectives. So sit back, relax, and let’s delve into the marvels of high-altitude medicine!
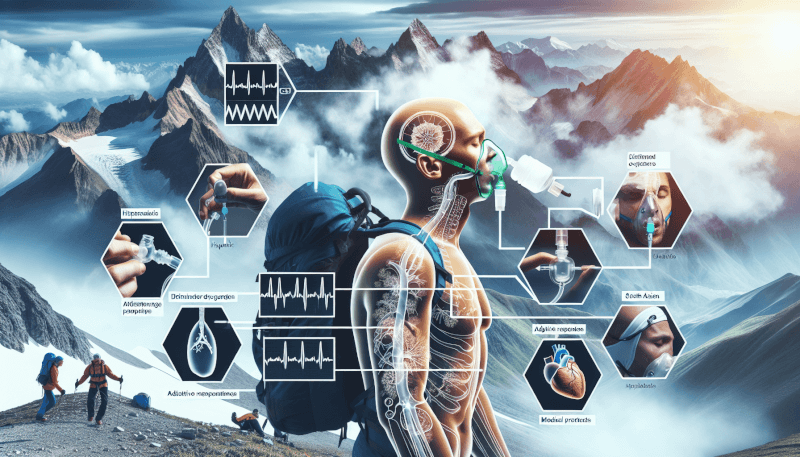
Physiological Changes at High Altitude
Hypoxemia
One of the fundamental physiological changes you’ll experience at high altitude is hypoxemia. Hypoxemia refers to reduced oxygen levels in your blood, primarily due to the lower oxygen partial pressure in the thin air at higher altitudes. This lack of oxygen triggers a series of adaptations in your body to enhance oxygen delivery to vital organs and tissues.
Hyperventilation
To compensate for the reduced oxygen levels, your body initiates hyperventilation at high altitude. This increased breathing rate helps you inhale more air and boosts oxygen uptake. You may notice yourself taking deeper and more rapid breaths, as your body efficiently pumps oxygen to meet the demands of your body’s tissues.
Fluid Shifts
Fluid balance in your body can be disrupted at high altitudes due to several factors. As you ascend, there is increased urine production and elevated fluid losses through respiration. Additionally, the lower atmospheric pressure can lead to fluid shift from your blood vessels into surrounding tissues. These fluid shifts can contribute to altitude-related illnesses and should be carefully managed.
Acute Mountain Sickness
Acute Mountain Sickness (AMS) is a common condition that many travelers experience when rapidly ascending to high altitudes. Symptoms of AMS may include headache, dizziness, nausea, fatigue, and difficulty sleeping. It’s important to acclimatize slowly to allow your body to adjust to the altitude and minimize the risk of AMS.
High-Altitude Pulmonary Edema
In severe cases, altitude sickness can progress to High-Altitude Pulmonary Edema (HAPE). HAPE occurs when fluid accumulates in the lungs, leading to breathing difficulties and decreased oxygen exchange. Prompt medical attention and descent to lower altitudes are vital for managing HAPE effectively.
High-Altitude Cerebral Edema
Another serious condition that can arise at high altitudes is High-Altitude Cerebral Edema (HACE). HACE involves swelling in the brain due to increased blood vessel permeability. Symptoms may include confusion, loss of coordination, severe headache, and even coma. Immediate descent and medical intervention are crucial for treating HACE.
Altitude Sickness and Treatment
Symptoms of Altitude Sickness
Recognizing the symptoms of altitude sickness is essential for early intervention and prevention of further complications. Headache, nausea, vomiting, dizziness, fatigue, and sleep disturbances are common tell-tale signs. It’s important to listen to your body and seek medical help if symptoms persist or worsen.
Acclimatization
The process of acclimatization allows your body to adjust gradually to higher altitudes, minimizing the risk of altitude sickness. It involves spending time at progressively higher altitudes, allowing your body to adapt to the reduced oxygen levels. Slow ascent and adequate rest are crucial for successful acclimatization.
Medications for Altitude Sickness
Certain medications can help prevent and alleviate altitude sickness symptoms. Acetazolamide, a diuretic, is often prescribed to stimulate breathing and decrease fluid accumulation. In severe cases, medications such as dexamethasone may be used to reduce brain and lung swelling. However, it is important to consult with a healthcare professional before taking any medication.
Effects of High Altitude on the Cardiovascular System
Increased Heart Rate
At higher altitudes, your heart has to work harder to supply oxygen to your body’s tissues. To compensate for the reduced oxygen availability, your heart rate increases, allowing for more efficient oxygen delivery. This increased heart rate is a normal physiological response to higher altitudes.
Elevated Blood Pressure
Another cardiovascular change at high altitude is a rise in blood pressure. The constricted blood vessels and increased sympathetic nervous system activity contribute to the elevation in blood pressure. However, these adaptations are essential for maintaining adequate blood flow and oxygen delivery to vital organs.
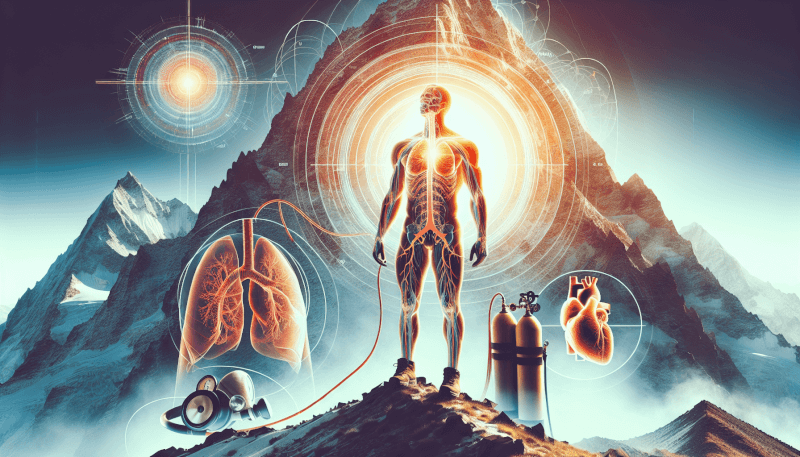
Increased Blood Volume
To compensate for the reduced oxygen-carrying capacity of the blood at high altitudes, your body increases the production of red blood cells. This process, known as polycythemia, helps enhance oxygen-carrying capacity and improves oxygen delivery to tissues. The increased blood volume also aids in maintaining adequate circulation.
Cardiac Output Changes
Cardiac output, the amount of blood pumped by your heart per minute, undergoes alterations at high altitude. Initially, cardiac output increases to meet the oxygen demands of your body. However, over time, it may decrease due to a combination of factors, including reduced blood volume and increased systemic vascular resistance.
Impaired Oxygen Delivery
Despite the body’s compensatory mechanisms, the reduced oxygen pressure at high altitude can still result in impaired oxygen delivery to tissues. This can lead to symptoms such as fatigue, weakness, and a decreased ability to perform physical activities. Adequate acclimatization and medical interventions can help mitigate these effects.

Effects of High Altitude on the Respiratory System
Hyperventilation
As mentioned earlier, hyperventilation is a critical response of the respiratory system to high altitude. The increased ventilation enables you to take in more oxygen and remove carbon dioxide efficiently. While this hyperventilation helps combat hypoxemia, it can also lead to respiratory alkalosis, a condition characterized by decreased levels of carbon dioxide in the blood.
Pulmonary Vasoconstriction
At high altitudes, the blood vessels in your lungs constrict as a protective mechanism to match oxygen delivery with the available supply. This phenomenon, known as hypoxic pulmonary vasoconstriction, redirects blood flow to well-aerated areas of the lungs. While it helps maintain oxygenation, it can also increase pulmonary arterial pressure and contribute to cardiovascular changes.
Reduced Oxygen Saturation
Due to the lower oxygen partial pressure at high altitude, your blood’s oxygen saturation levels decrease. This means that a smaller fraction of your red blood cells is carrying oxygen, further exacerbating the physiological challenges of delivering oxygen to tissues. Monitoring oxygen saturation levels using pulse oximeters is often recommended in high-altitude settings.
Respiratory Acidosis
In some cases, prolonged exposure to high altitudes may lead to respiratory acidosis, a condition characterized by increased carbon dioxide levels and decreased blood pH. This can occur if your body’s compensatory mechanisms fail to maintain proper acid-base balance. Respiratory acidosis requires medical attention and proper management to prevent further complications.
Hypoxic Training and Performance
Hypoxia and Athlete Performance
High-altitude training and exposure to hypoxia have long been an interest in the realm of athlete performance enhancement. Exposing athletes to high-altitude environments or using simulated hypoxic training methods can trigger adaptations in the body, such as increased red blood cell production and improved oxygen utilization. These adaptations can potentially enhance endurance and performance in athletes.
Altitude Training Methods
Altitude training methods include living and training at high altitudes or utilizing altitude simulation techniques. Living at high altitudes for extended periods allows athletes to experience the physiological adaptations associated with hypoxia. Altitude simulation systems, such as oxygen tents or hypoxic chambers, can replicate the reduced oxygen conditions without the need for constant travel to high-altitude locations.
Benefits of Hypoxic Training
Hypoxic training can provide numerous benefits to athletes, including improved oxygen utilization, increased lactate threshold, enhanced cardiorespiratory function, and better overall endurance performance. However, it’s crucial to note that hypoxic training should be supervised by qualified professionals to ensure safety and optimize training outcomes.

Preventing Altitude-Related Illnesses
Gradual Ascent
One of the most effective preventive measures against altitude-related illnesses is a gradual ascent. Ascending slowly allows your body to acclimatize and adapt to the changing altitude. Rapid ascents significantly increase the risk of altitude sickness, so it’s vital to plan your journey accordingly and factor in appropriate rest days to adjust to higher altitudes.
Proper Hydration
Staying properly hydrated is essential at high altitudes. Dehydration can exacerbate the symptoms of altitude sickness and hinder acclimatization. Make sure to drink plenty of fluids throughout the day, even if you don’t feel thirsty. Avoid excessive alcohol consumption, as it can contribute to dehydration and further compromise your body’s ability to adapt to high altitudes.
Avoidance of Alcohol and Smoking
In addition to staying hydrated, it’s crucial to avoid alcohol and smoking at high altitudes. Both alcohol and smoking can impair oxygen delivery and compromise respiratory function. They can also exacerbate the symptoms of altitude sickness and increase the risk of complications. Opt for healthier choices that promote optimal oxygen transport in your body.
Use of Acetazolamide
Acetazolamide, a medication mentioned earlier, can be used as a preventive measure for altitude sickness. This diuretic helps stimulate breathing and reduces fluid accumulation in your body. It’s important to consult with a healthcare professional before using acetazolamide, as they can provide proper guidance and recommendations based on your individual circumstances.
Medical Considerations for High-Altitude Travelers
Pre-Existing Medical Conditions
If you have pre-existing medical conditions, it’s essential to consult with your healthcare provider before traveling to high-altitude regions. Certain medical conditions, such as heart or lung diseases, may increase the risk of complications at high altitudes. Your healthcare provider can assess your condition, provide necessary advice, and recommend appropriate precautions to ensure your safety.
Altitude and Pregnancy
Pregnant women should be cautious when traveling to high-altitude locations. The reduced oxygen levels can affect both the mother and the developing fetus. It’s generally recommended to avoid altitudes above 3,000 meters (9,800 feet) during pregnancy. If unavoidable, consult with your obstetrician to assess the potential risks and develop an individualized plan.
Altitude and Children
Children can experience altitude sickness and related conditions just like adults. It’s important to be vigilant and monitor children’s symptoms closely if traveling to high altitudes with them. Adequate hydration, proper acclimatization, and close medical supervision are particularly crucial for the well-being of children in high-altitude settings.
High-Altitude Emergency Situations
High-Altitude Rescue
In the event of an emergency situation at high altitude, it’s important to know how to seek help effectively. High-altitude rescues often require specialized teams and equipment, considering the challenging environmental conditions. It’s crucial to have access to means of communication, such as satellite phones or emergency locator beacons, to alert rescue services promptly.
First Aid for Altitude Sickness
If someone in your group experiences altitude sickness symptoms, there are several immediate first aid measures you can take while waiting for professional medical assistance. These include ensuring adequate rest, providing plenty of fluids, administering medication if advised by a healthcare professional, and monitoring the individual’s condition closely until medical help arrives.
Emergency Oxygen Therapy
In severe cases of altitude sickness, emergency oxygen therapy may be necessary. Oxygen can help alleviate symptoms and stabilize vital signs, providing temporary relief before descending to lower altitudes. Emergency oxygen cylinders and masks should be readily available in high-altitude settings, especially in remote or isolated areas.
Future Perspectives in High-Altitude Medicine
Research on Genetic Factors
The field of high-altitude medicine is continually evolving, and ongoing research focuses on understanding the genetic factors that contribute to an individual’s susceptibility to altitude-related illnesses. Identifying specific genes and genetic variations can lead to personalized interventions and targeted preventive measures, improving the overall management of high-altitude conditions.
Artificial Altitude Environments
Artificial altitude environments, such as hypobaric chambers, have emerged as valuable tools for research, training, and medical interventions. These controlled environments replicate the reduced oxygen conditions at high altitudes, allowing for studying physiological responses and developing innovative strategies for altitude-related challenges.
Enhancing Oxygen Delivery
Efforts are being made to develop new techniques and interventions for enhancing oxygen delivery to tissues at high altitudes. Innovations such as oxygen-carrying blood substitutes, pharmaceutical agents, and advanced medical devices all hold promise in improving oxygen transport and mitigating the physiological limitations experienced at high elevations.
In conclusion, understanding the complex realm of high-altitude medicine and physiology is crucial for anyone venturing to lofty heights. From the physiological changes that occur in your body to the various altitude-related illnesses and their treatments, this article has covered a comprehensive range of topics. By taking preventive measures, acclimatizing wisely, and seeking appropriate medical advice, you can ensure a safe and enjoyable journey in high-altitude regions. So, embrace the wonders of the mountains and set out on your high-altitude adventure with confidence, knowing that you’re well-informed and prepared for this exhilarating experience!